

This training should focus on the principles of early intervention, meticulous planning, vigilant infection control, efficient processes, clear communication and standardised practice.Īn outbreak in Wuhan, China, in 2019 of the novel coronavirus named severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) (formerly called HCoV‐19) has led to a pandemic of coronavirus disease 2019 (COVID‐19).
Safe, simple, familiar, reliable and robust practices should be adopted for all episodes of airway management for patients with COVID‐19.Ĭhanges in management as a result of this statement: Airway clinicians in Australia and New Zealand should now already be involved in regular intensive training for the airway management of the COVID‐19 patient group.The principles for airway management should be the same for all patients with COVID‐19 (asymptomatic, mild or critically unwell).
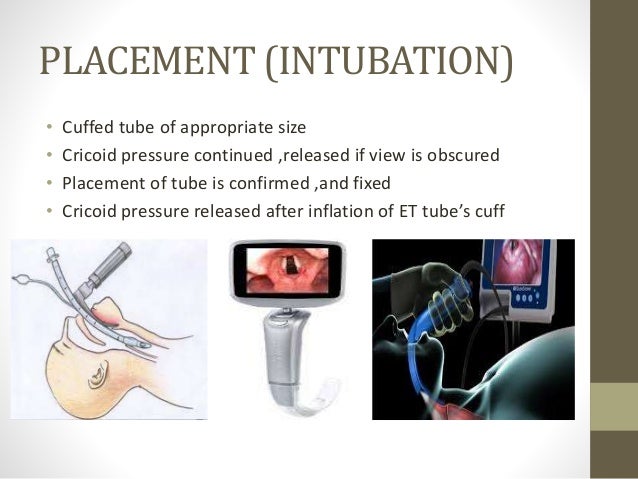

Significant institutional preparation is required to optimise staff and patient safety in preparing for the airway management of the COVID‐19 patient group.Early intubation should be considered to prevent the additional risk to staff of emergency intubation and to avoid prolonged use of high flow nasal oxygen or non‐invasive ventilation.Consideration should be given to using a checklist that has been specifically modified for the COVID‐19 patient group.They should be followed where they do not contradict our specific recommendations for the COVID‐19 patient group. Generic guidelines exist for the intubation of different patient groups, as do resources to facilitate airway rescue and transition to the “can't intubate, can't oxygenate” scenario.It has been widely endorsed by relevant specialty colleges and societies. Introduction: This statement was planned on 11 March 2020 to provide clinical guidance and aid staff preparation for the coronavirus disease 2019 (COVID‐19) pandemic in Australia and New Zealand. Statistics, epidemiology and research design.Quality review and patient monitoring should be addressed when policies about RSI are developed in the ED.Neuromuscular blocking agents and appropriate sedative and induction agents should be immediately available in the ED and accessible to all physicians who perform RSI in the ED.Physicians performing RSI should possess training, knowledge, and experience in the techniques and pharmacologic agents used to perform RSI.The American College of Emergency Physicians recognizes the role of RSI in modern emergency care and supports the following principles. The technique includes specific protection against aspiration of gastric contents, provides excellent access to the airway for intubation, and permits pharmacologic control of adverse responses to illness, injury, and the intubation itself. RSI is defined as a technique where a potent sedative or induction agent is administered virtually simultaneously with a paralyzing dose of a neuromuscular blocking agent to facilitate rapid tracheal intubation. Rapid-sequence intubation (RSI) is an important technique for airway management of patients in the emergency department and is in the domain of emergency medicine practice. Reaffirmed February 2018, April 2012, October 2006, October 2000


 0 kommentar(er)
0 kommentar(er)
